Carotid-cavernous fistula
Carotid-cavernous fistulae are abnormal communications between the carotid arteries (ICA and ECA) and venous compartments of the cavernous sinus.
Carotid artery cavernous fistulas can be classified in two ways: as “direct,†consisting of a tear in the wall of the cavernous ICA causing an arteriovenous communication with the cavernous sinus; or as “indirect,†which is synonymous with a DAVF in communication with the cavernous sinus.
Direct CACFs may be spontaneous or acquired lesions. Closed head injury in which the base of the skull has fractured and the ICA sheared from its dural attachment are the most common cause of this lesion. The cavernous portion of the internal carotid artery is fixed to the dura at the entry point at the petrous opening into the sinus and exit at the anterior clinoid process. At the time of the injury, the artery is hence exposed to shearing forces leading to laceration and rupture.
Alternative origins include rupture of an intracavernous ICA aneurysm, iatrogenic injury during transsphenoidal pituitary resection, fibromuscular dysplasia, or collagen vascular diseases such as Marfan syndrome and Ehlers–Danlos syndrome.
Classification :
Based on angiographic findings, CCFs are categorized into 4 types :
Type A fistulas consist of a direct connection between the intracavernous internal carotid artery and the cavernous sinus. They usually are high-flow and high-pressure fistulas.
Type B fistulas consist of a dural shunt between intracavernous branches of the internal carotid artery and the cavernous sinus.
Type C fistulas consist of a dural shunt between meningeal branches of the external carotid artery and the cavernous sinus.
Type D fistulas are a combination of types B and C, with dural shunts between internal and external carotid artery branches and the cavernous sinus.
Types B, C, and D tend to be lower-flow and lower-pressure fistulas with a slower progression of signs and symptoms and higher incidence of spontaneous resolution.
A caroticocavernous fistula results in high-pressure arterial blood entering the low-pressure venous cavernous sinus. This interferes with normal venous drainage patterns and compromises blood flow within the cavernous sinus and the orbit.
Clinical Presentation :
Carotid artery cavernous fistulas may present with ophthalmoplegia, proptosis, chemosis, pain, and reduced visual acuity.
Direct irritation or associated trauma to the cranial nerves traversing the cavernous sinus can result in third, fourth, fifth, and sixth nerve palsies.
Retrograde flow of arterialized blood through the superior and inferior ophthalmic veins into the orbit may cause proptosis, chemosis, pain, and reduced visual acuity.
Retinal perfusion pressure can be compromised to the extent of inducing permanent blindness. These ocular symptoms may be exacerbated by hypoplasia or thrombosis/occlusion of the inferior petrosal sinuses that can occur as a result of prolonged arteriovenous artery–vein communication.
Diagnosis:
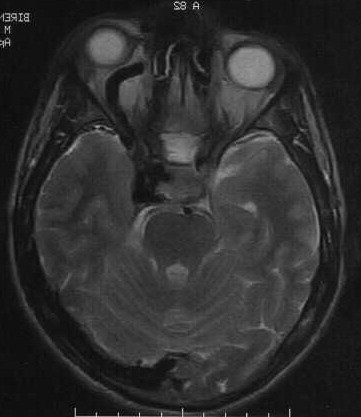
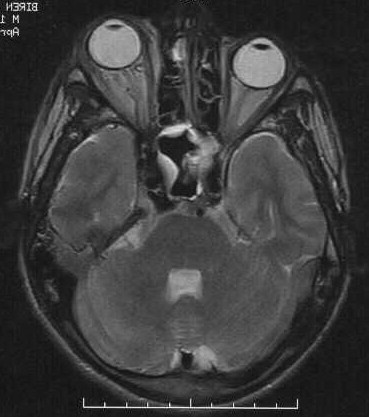
CT/MRI :
The findings are the effects rather than the fistula itself.
1. Proptosis is noted on the affected side.
2. There is engorgement of the ophthalmic veins and extra ocular muscle congestion.
3. A markedly enhancing cavernous sinus is seen bulging outwards.
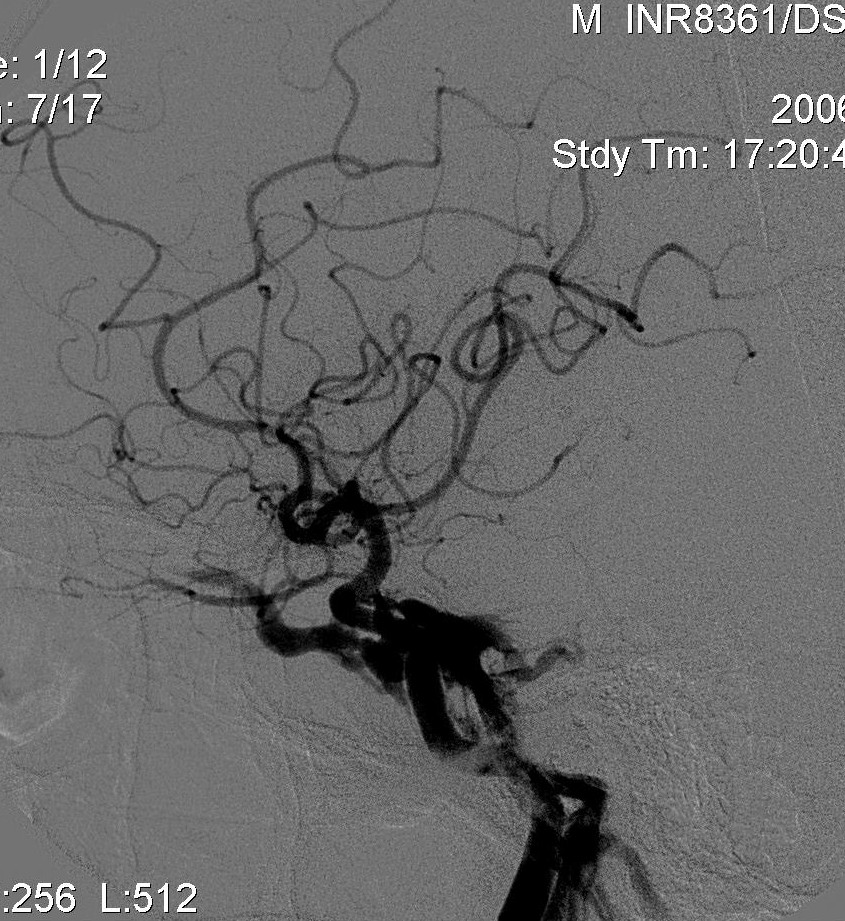
Angiography:
Angiography:
Diagnostic angiography can demonstrate
1. the fistula and differentiates between a dural and direct CCF .
2. the severity of arteriovenous communication,
3. Extent of intracerebral collateral pathways,
4. Residual antegrade flow in the ICA beyond the fistula.
Treatment:
Intraocular pressures exceeding 40 mm Hg or rapidly progressive visual deterioration are indications for emergency therapy to avoid permanent loss of vision.
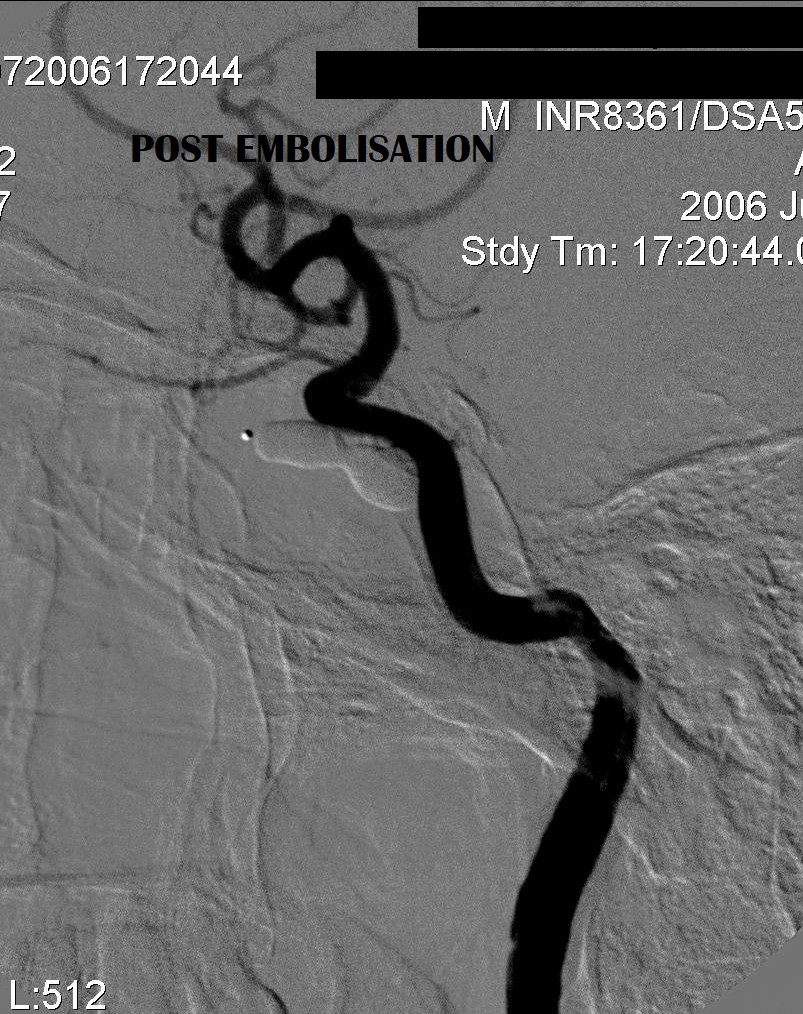
The goal of treatment is to eliminate the fistula and preserve the carotid artery patency.
Transarterial–transfistula balloon embolization for direct- type fistulas and transvenous coil embolization of indirect fistulas are often curative.
The preferred endovascular procedure is transarteral– transfistula balloon embolization. The detachable balloon is navigated across the fistula onto the venous side and inflated in the cavernous sinus to occlude the rent in the artery thus sealing off the fistula.
If transarterial–transfistula balloon occlusion is not feasible, transvenous coil embolization may be performed using a microcatheter positioned in the cavernous sinus via the inferior petrosal sinus. Although detachable coils have the advantage of being able to be repositioned or removed if placement is unsatisfactory, they are significantly more expensive and less thrombogenic than pushable fibered coils.
When using either balloons or coils, however, it is important not to redirect or increase venous drainage into the ophthalmic or cortical veins, because this may aggravate ocular symptoms or precipitate intracranial hemorrhage.
Certain fistulas cannot be completely occluded without parent vessel sacrifice. Sacrifice of the ICA may be considered only if adequate intracranial collateral pathways exist.
Conservative treatment for indirect CACFs consists of self-applied CA compression by using the contralateral hand every 30 minutes for 1-minute intervals during waking hours. By compressing the CA sheath contents, antegrade flow is diminished and venous pressure elevated, promoting thrombosis of the fistula.
RESULTS OF ENDOVASCULAR TREATMENT
Chemosis and proptosis typically improve rapidly after successful obliteration of CACFs. Visual acuity and ophthalmoplegia may take longer to resolve and can be exacerbated in the short term by thrombosis and associated swelling within the cavernous sinus.