EPIDERMOID
INTRODUCTION:
An epidermoid tumor is a benign (i.e., non-cancerous) neoplasm of the brain. Both congenital and acquired epidermoid cysts occur. They account for approximately 1% of all intracranial tumors. Although these lesions are congenital, patients are usually not symptomatic until they are aged 20-40 years. They usually occur in the cerebellopontine angle (CPA) or parasellar region. They can also be found on the brain stem in extremely rare instances.
PATHOPHYSIOLOGY:
PATHOPHYSIOLOGY:
Congenital epidermoid “tumor†is actually a nonneoplastic inclusion cyst. Epidermoid cysts probably arise from inclusion of ectodermal epithelial elements at the time of neural tube closure or during formation of the secondary cerebral vesicles.
Acquired epidermoid cysts develop as a result of trauma. In this case, epidermis is implanted into deeper underlying tissues and forms a cyst that continues to desquamate keratin.
Epidermoids should be distinguished from dermoids, which also are a result of congenital ectodermal inclusion. Dermoid inclusion cysts also result from ectodermal inclusions, but they have a lining that has further differentiated to include dermal appendage structures such as hair follicles, sebaceous glands, and sweat glands.
ANATOMY:
Although the vast majority of epidermoids are intradural, they can be extra dural. The most common locations are within the cerebellopontine (CP) angle, parasellar region, and middle cranial fossa. The CP angle is the most common site for epidermoids. Of all CP angle masses epidermoids are the third most common after vestibular scwannomas and meningiomas. At diagnosis epidermoids usually insinuate within the sulci and cisterns and they may engulf cranial nerves and blood vessels.
CLINICAL FEATURES:
The clinical presentation depends upon the location of the mass. Common presentations for CP angle masses include
1) Headache
2) Diplopia
3) Trigeminal neuralgia
4) Hypoacusia
5) Gait ataxia.
IMAGING FEATURES:
MRI imaging is most reliable study in diagnosing Epidermoids. The extent of disease is well depicted; this depiction facilitates surgical planning.
Findings. On T1-weighted images these lesions are generally slightly hyperintense or isointense relative to gray matter. More specifically, the T1-weighted signal intensity tends to vary with the lipid content, with the signal intensity being increased in lesions with high lipid content and decreased in those with low lipid content. The lesions are usually isointense relative to CSF on T2-weighted images, but they may be slightly hyperintense. The center of these lesions usually has an internal architecture with areas of heterogeneity.
Enhancement of portions of the rim may be seen after the administration of contrast material. The remainder of the lesion does not enhance. Proton density–weighted and then fluid-attenuated inversion recovery (FLAIR) images were first used to differentiate epidermoids from arachnoid cysts. These sequences demonstrate epidermoids as being hyperintense relative to CSF.
Now, diffusion-weighted imaging can be used to differentiate these entities, because epidermoids have markedly restricted diffusion and, therefore, high signal intensity on the diffusion-weighted trace images. The free water in arachnoid cysts has low signal intensity. Diffusion-weighted images are helpful in assessing residual epidermoid tumors after surgical resection.
Degree of Confidence: MRI findings allow diagnosis with a high degree of confidence.
CT findings may be nonspecific and is not as reliable as MRI.
Findings On CT-scans, epidermoid lesions with decreased attenuation are most often extradural. They usually has the same attenuation as that of cerebrospinal fluid (CSF); these characteristic makes their differentiation from arachnoid cysts difficult. Enhancement is rare, but can sometimes be seen around the margin of the tumor. Calcification occurs in only 15-20% of cases.
DIFFERENTIAL DIAGNOSIS:
1) Arachnoid cyst.
2) Cystic schwannomas.
3) Malignant transformation.
TREATMENT:
A sub-total resection of the tumor.
In our case:
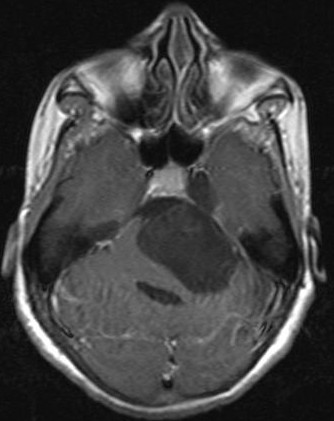
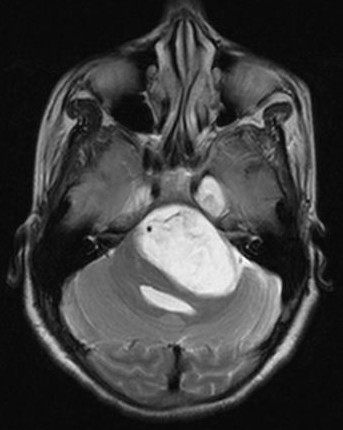
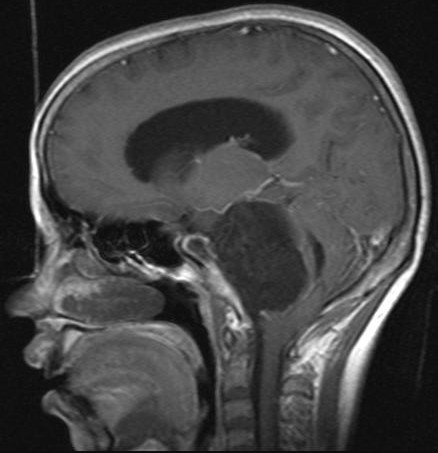
MRI Imaging features are:
Epidermoid is seen in the left CP angle cistern. It follows CSF signal intensity on T1 and T2WI, but not on the FLAIR images and displays restricted diffusion.
Tumor is causing severe compression of the adjacent brainstem. Due to mass effect there is compression of the IV ventricle resulting in dilatation of the lateral and third ventricles along with the trans ependymal CSF migration. Inferior tonsillar herniation is seen.
Imaging features are suggestive of Left CPA cistern Epidermoid.