ALLERGIC BRONCHOPULMONARY ASPERGILLOSIS.
Pulmonary aspergillosis is a spectrum of mycotic diseases caused by Aspergillus species, usually Aspergillus fumigatus. This intensely antigenic and ubiquitous soil fungus is commonly found in the sputum of healthy individuals. However, in susceptible hosts, its ability to invade the arteries and veins facilitates its hematogenous spread.
Pulmonary aspergillosis may take any of 4 forms:
- Allergic bronchopulmonary aspergillosis (ABPA) is caused by a hypersensitivity reaction to the fungus and most commonly occurs in those with asthma.
- Saprophytic aspergillosis, or aspergilloma, is the most common form. This form is noninvasive and involves colonization of preexisting cavities.
- Chronic necrotizing aspergillosis, also called airway-invasive or semi-invasive aspergillosis, is a chronic cavitary pneumonic illness that often affect patients with preexisting chronic lung disease.
- Angioinvasive aspergillosis affects immunocompromised patients and is often fatal.
The primary diagnostic criteria for ABPA include the following:
- Asthma, 84-96%
- Blood eosinophilia, 8-40%
- Elevated serum IgE levels
- Positive skin test results for A fumigatus
- Elevated serum levels of IgE and IgG specific for A fumigatus
- Presence of precipitating antibodies to A fumigatus
The primary radiologic criteria include fixed or transitory pulmonary infiltrates and central bronchiectasis as a late manifestation. A set of secondary criteria can sometimes be applied; these include the presence of A fumigatusmycelia in the sputum, the expectoration of brown sputum plugs, and a delayed cutaneous reaction to A fumigatus antigen.
ABPA can be staged by using the following clinical and radiologic criteria:
- Stage I - Acute presentation with 6 of the 8 primary diagnostic criteria listed above
- Stage II - Resolving pulmonary infiltrates with decreasing IgE levels leading to remission
- Stage III - Recurrence of acute symptoms after a period of remission
- Stage IV - Steroid dependency
- Stage V - Irreversible lung damage leading to fibrosis
X- Ray Findings: In ABPA, chest radiographic appearances include the following: (1) fleeting alveolar subsegmental or lobar infiltrates, which are usually bilateral (65%) and predominant in the upper lobes (50%); (2) central 1-2-cm ring shadows that represent varicose or cystic bronchiectasis; and (3) tram-link bronchial walls due to edema. The second-order bronchi may become plugged with mucus, and they may be visible as 2.5-6-com long V- or Y-shaped branching tubular opacities that may grow over time and persist for months; this is the so-called finger-in-glove sign.
Other features include lobar consolidation, atelectasis, postobstructive pneumonia, cavitation, air trapping, and parenchymal scarring or fibrosis, all of which are more pronounced in the upper lobes. Focal pleural thickening is also reported. Occasionally, mycetomas develop in ectatic bronchi.
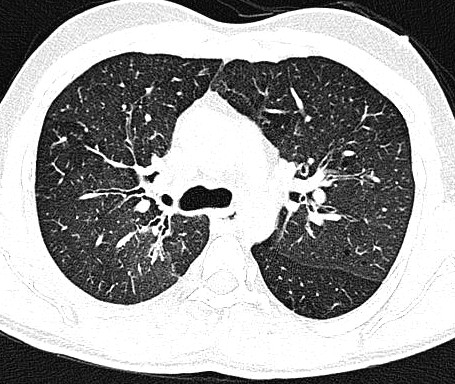
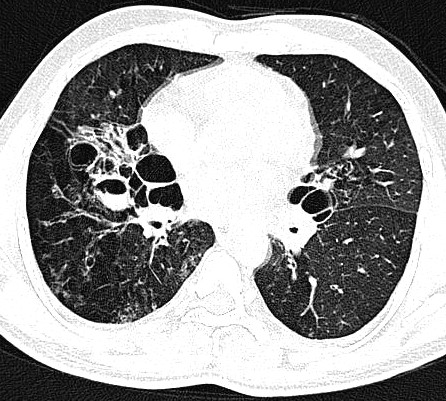
CT Findings: Bronchiectasis and peribronchial thickening are the most common CT findings in ABPA. Appearances tend to be more severe than in those of chronic uncomplicated asthma. ABPA typically involves the segmental and subsegmental bronchi, particularly those in the upper lobes. However, recent studies have shown that central bronchiectasis simply indicates long-standing severe inflammation; as a marker, it is not as specific for ABPA as was once thought.
High-attenuating mucoid impaction, present in as many as 30% of patients, is a characteristic finding. Occasionally, lobar or segmental atelectasis may be a feature. Mucus plugging of the small airways can be observed on high-resolution CT scans, with resultant centrilobular nodularity and the tree-in-bud sign. Abnormalities of lung attenuation due to either mosaic perfusion or air trapping may also be identified. Scans obtained during expiration are useful in differentiating the findings in this instance