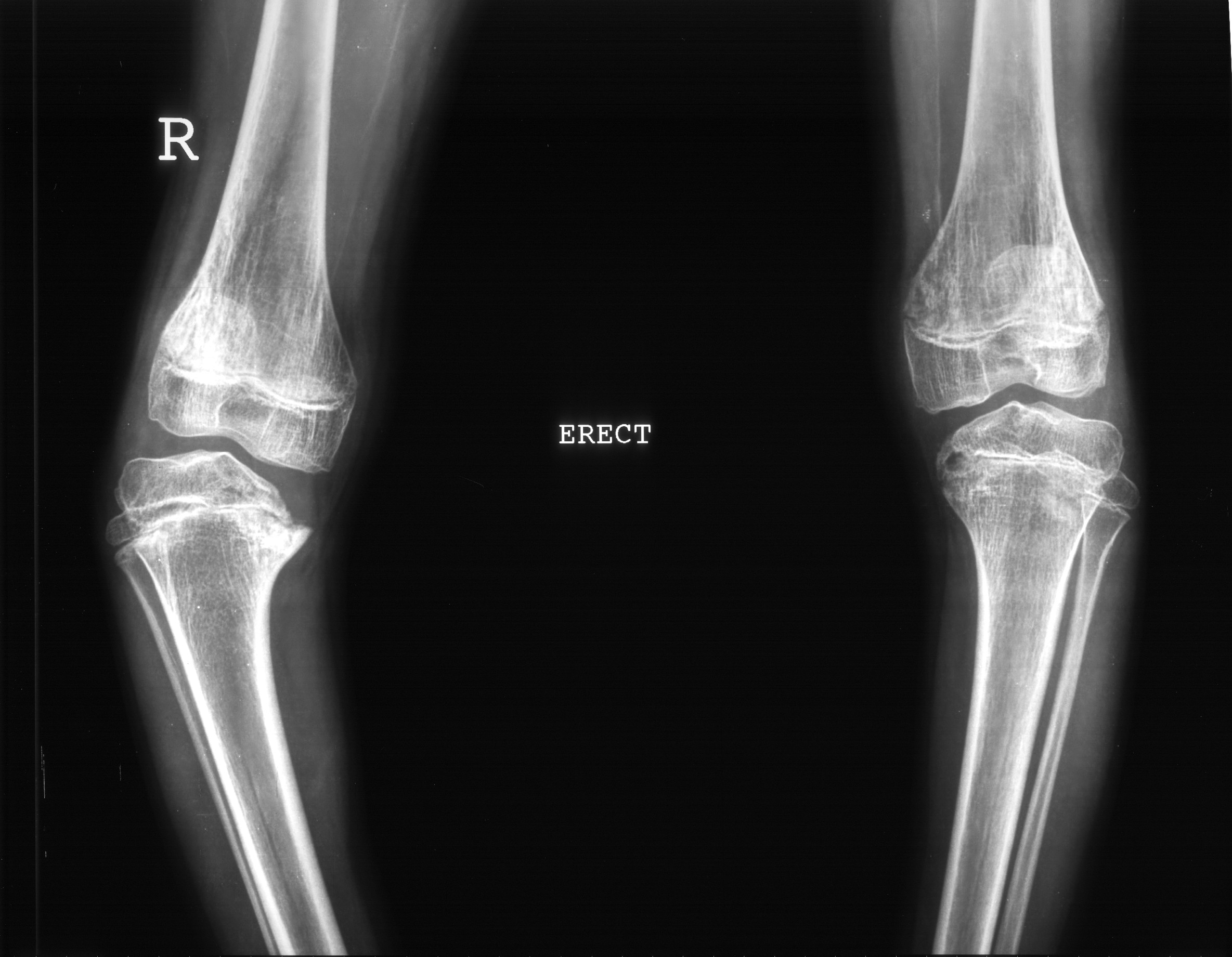
Diagnosis - Bilateral Blounts disease ( Right > Left) with Varus deformity of the Right leg.
Blount disease is an uncommon growth disorder characterized by disordered ossification of the medial aspect of the proximal tibial physis, epiphysis, and metaphysis. This progressive deformity is manifested by varus angulation and internal rotation of the tibia in the proximal metaphyseal region immediately below the knee. The natural history of this disease leads to irreversible pathologic changes, especially at the medial portion of the proximal tibial epiphysis because of growth disturbances of the subjacent physis.
Blount disease can occur in growing children of any age and is classified into 2 groups (ie, early onset and late onset). Early onset (in children <3 y) is termed the infantile type. The late-onset group includes the juvenile form (in children aged 4-10 y) and adolescent form (in those aged 11 years and older) of the disease.
Pathophysiology:
The common denominator in tibia vara cases is abnormal stress placed on the posteromedial proximal tibial epiphysis that leads to growth suppression. Predisposing factors for the development of the condition include obesity, early walking, and black ancestry. Black children have been noted to have excessive ligamentous laxity, and they begin to walk at an earlier age. Both of these factors predispose them to Blount disease. Obesity and early walking exaggerate the impact of physiologic bowing and increase the stress placed on the physis of the proximal tibia.
As a result, altered mechanical forces in the proximal tibia lead to abnormal axial loading, which results in a change in direction of the weight-bearing forces from the perpendicular to the oblique. The oblique angle tends to displace the tibial epiphysis in a lateral direction, overloading the posteromedial segment and inhibiting its growth. A cycle of further longitudinal growth is established, and this results in progressive varus deformity. Therefore, unless the disease is diagnosed and treated early, the condition progressively worsens.
X- Ray Findings: Radiography is the primary modality used to diagnose tibia vara.
X-ray findings primarily involve the posteromedial parts of the proximal tibial epiphysis, growth plate, and the metaphysis. A standing anteroposterior radiograph of both legs is used to demonstrate bowing and abnormality at the medial aspect of the proximal tibia. In more advanced cases, bowing is seen at both ends of the tibia. On lateral knee radiographs, a posteriorly directed projection at the proximal tibial metaphyseal level is seen.
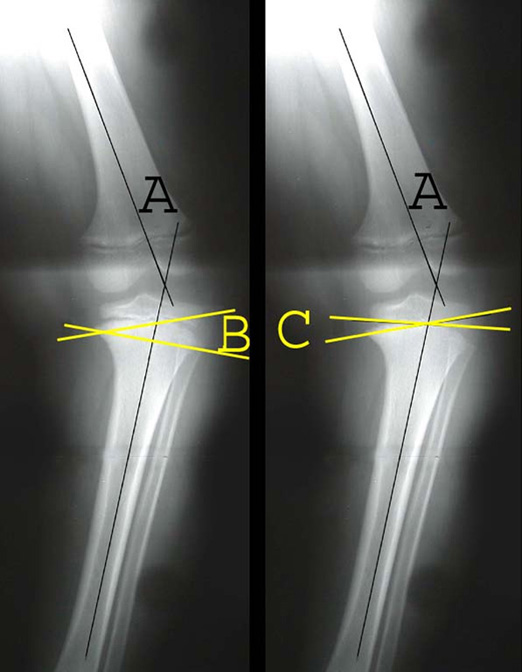
Different radiologic measurements have been used in an attempt to confirm the presence of the disease. The femoral-tibial angle helps confirm the varus position of the leg, but it can be misleading secondary to the rotation of the leg, which may be positional or due to a coexisting rotational abnormality.
Early changes of infantile Blount disease can be made by measuring the metaphyseal-diaphyseal angle of the proximal tibia, that angle formed by the intersection of a line through the transverse plane of the proximal tibial metaphysis with a line perpendicular to the long axis of the tibial diaphysis.
The severity of the varus deformity is based on determination of the tibiofemoral angle as measured on standing anteroposterior radiographs that include the ankle, knee, and most of the femur; the metaphyseal-diaphyseal angle; and the metaphyseal-epiphyseal angle, that angle formed by intersection of a line through the transverse plane of the proximal tibia epiphysis with a line through the transverse plane of the metaphysis.
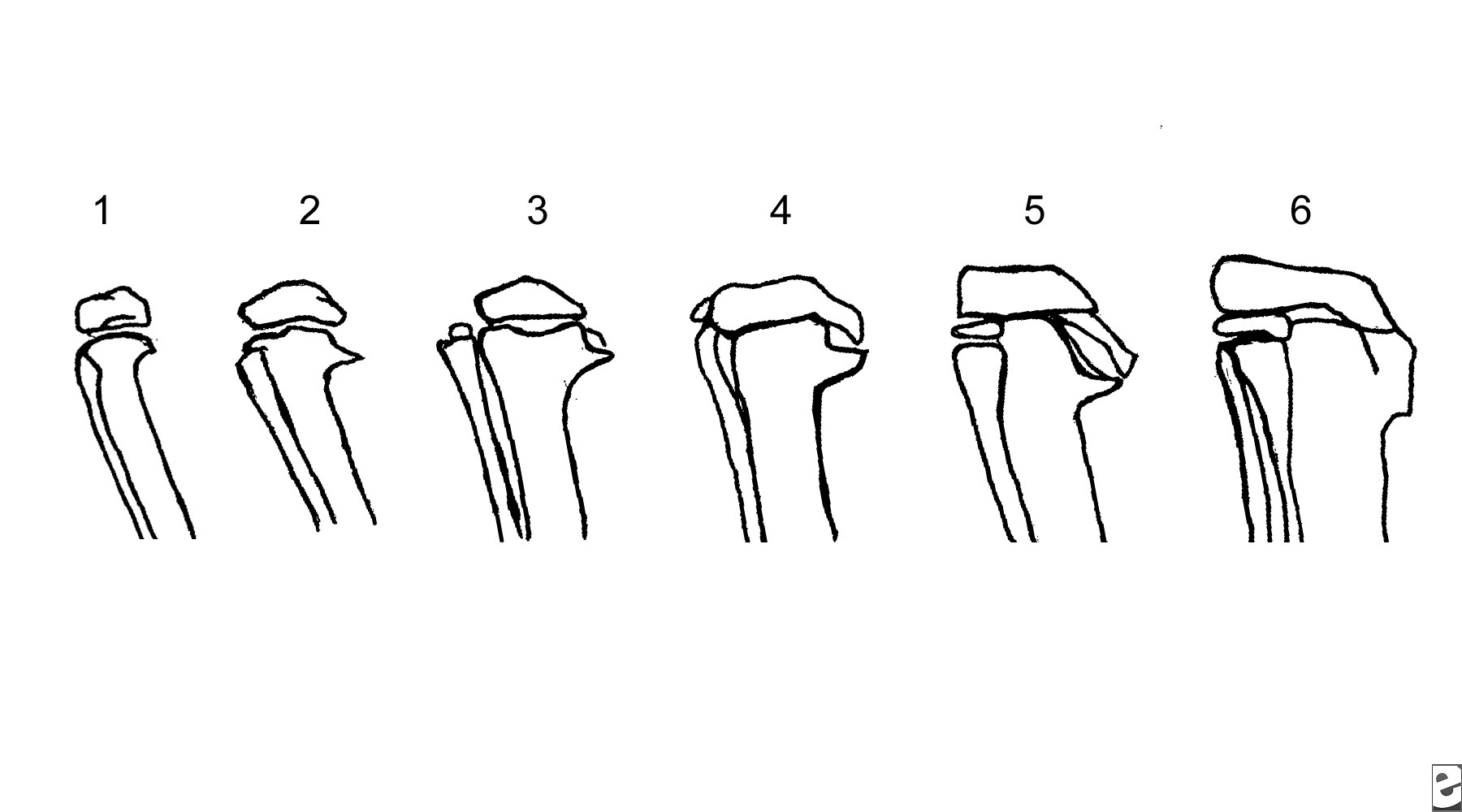
In 1952, Langenskiold first proposed a 6-stage classification of radiographic changes. This remains the most commonly used system .
In 1952, Langenskiold first proposed a 6-stage classification of radiographic changes. This remains the most commonly used system .
Depiction of the 6 stages of the Langenskiold classification of tibia vara, as they would be seen on radiographs.
MRI Findings: Although radiographic findings in Blount disease usually are diagnostic, MRI has the advantage of direct depiction of the epiphysis and the growth plate. How MRI can aid in evaluation and treatment of patients with Blount disease is debatable. MRI has a distinct advantage in a subset of patients with advanced or recurrent tibia vara. In these patients, MRI can demonstrate the extent of the physeal bar to quantify the percentage of physeal involvement. An open physis is bright on a T2-weighted MRI. The physeal bar appears black on a T2-weighted image. Early physeal fusion of the medial proximal tibial and, less frequently, medial distal femoral physis can occur from the injury of chronic weight bearing. This injury can lead to progressive genu varus from medial tethering of the growth plates. Removal of the physis medially may help restore normal growth.
MRI Findings: Although radiographic findings in Blount disease usually are diagnostic, MRI has the advantage of direct depiction of the epiphysis and the growth plate. How MRI can aid in evaluation and treatment of patients with Blount disease is debatable. MRI has a distinct advantage in a subset of patients with advanced or recurrent tibia vara. In these patients, MRI can demonstrate the extent of the physeal bar to quantify the percentage of physeal involvement. An open physis is bright on a T2-weighted MRI. The physeal bar appears black on a T2-weighted image. Early physeal fusion of the medial proximal tibial and, less frequently, medial distal femoral physis can occur from the injury of chronic weight bearing. This injury can lead to progressive genu varus from medial tethering of the growth plates. Removal of the physis medially may help restore normal growth.
A recent article about MRI changes in bowleg deformities of early infancy suggested a possible role for MRI in differentiating physiologic bowing from Blount disease. Children who eventually had Blount disease were found to have a depression of the medial physis and abnormal signal intensity in the metaphysis in addition to the lesion in the epiphysis. In comparison, children with physiologic bowing were found to have high signal intensity only in the epiphyseal cartilage. However, most patients with combined changes did not develop Blount disease